Bursitis Ball Of Foot Cure
Bursae (two or more bursa) are small, fluid-filled sacs that cushion the bones, tendons and muscles surrounding your joints. They contain a lubricating fluid that reduces friction, allowing tissues in the body to glide past each other smoothly. Imagine the bursa as a protective layer that helps keep a tendon or muscle from fraying or getting aggravated as it eases over a bone or around a corner. Bursitis is a condition that occurs when a bursa becomes inflamed: irritated, red and filled with more fluid than normal.
Causes
There are several factors which can lead to a person developing retrocalcaneal bursitis. In athletes, especially runners, overtraining, sudden excessive increase in running mileage may lead to retrocalcaneal bursitis. Tight or ill-fitting shoes can be another causative factor as they can produce excessive pressure at the back of the heel due to restrictive heel counter. A person with an excessively prominent posterosuperior aspect of the heel bone (Haglund deformity) may also have a higher predisposition to retrocalcaneal bursitis. In such individuals, pain would be reproduced when the ankle goes into dorsiflexion.
Symptoms
Unlike Achilles tendinitis, which tends to manifest itself slightly higher on the lower leg, Achilles tendon bursitis usually creates pain and irritation at the back of the heel. Possible signs of bursitis of the Achilles tendon include difficulty to rise on toes. Standing on your toes or wearing high heels may increase the heel pain. Inflammation and tenderness. The skin around your heel can become swollen and warm to the touch. Redness may be visible. Pain in the heel. Pain tends to become more prominent when walking, running, or touching the inflamed area. Stiffness. The back of your ankle may feel a little stiff due to the swelling of the bursa.
Diagnosis
After you have described your foot symptoms, your doctor will want to know more details about your pain, your medical history and lifestyle, including whether your pain is worse at specific times of the day or after specific activities. Any recent injury to the area. Your medical and orthopedic history, especially any history of diabetes, arthritis or injury to your foot or leg. Your age and occupation. Your recreational activities, including sports and exercise programs. The type of shoes you usually wear, how well they fit, and how frequently you buy a new pair.
Non Surgical Treatment
According to the National Institutes of Health, custom heel wedges can be purchased by people suffering from retrocalcaneal bursitis. These wedges reduce stress on the heel, which can reduce the pain and inflammation associated with an inflamed bursa. They can be purchased without a prescription, making it easy for anyone experiencing a flare-up of symptoms to get the added support of these wedges.
Surgical Treatment
Only if non-surgical attempts at treatment fail, will it make sense to consider surgery. Surgery for retrocalcanel bursitis can include many different procedures. Some of these include removal of the bursa, removing any excess bone at the back of the heel (calcaneal exostectomy), and occasionally detachment and re-attachment of the Achilles tendon. If the foot structure and shape of the heel bone is a primary cause of the bursitis, surgery to re-align the heel bone (calcaneal osteotomy) may be considered. Regardless of which exact surgery is planned, the goal is always to decrease pain and correct the deformity. The idea is to get you back to the activities that you really enjoy. Your foot and ankle surgeon will determine the exact surgical procedure that is most likely to correct the problem in your case. But if you have to have surgery, you can work together to develop a plan that will help assure success.
Hammer Toes Definition
 Overview
Overview
A Hammer toe is a toe that becomes permanently bent in the middle so that the end of the toe points downward. The portion of the toe before the joint where the bend occurs tends to arch upward. A hammer toe takes years to develop. Once the toe becomes permanently bent, corns or calluses may form. Treatment helps control symptoms in many people, but surgery is sometimes needed to straighten the toe.
Causes
It is possible to be born with a hammer toe, however many people develop the deformity later in life. Common causes include tightened tendons that cause the toe to curl downward. Nerve injuries or problems with the spinal cord. Stubbing, jamming or breaking a toe. Having a stroke. Being a diabetic. Having a second toe that is longer than the big toe. Wearing high heels or tight shoes that crowd the toes and don?t allow them to lie flat. Aging.
The most obvious sign of hammertoes are bent toes, other symptoms may include pain and stiffness during movement of the toe. Painful corns hammertoes on the tops of the toe or toes from rubbing against the top of the shoe's toe box. Painful calluses on the bottoms of the toe or toes. Pain on the bottom of the ball of the foot. Redness and swelling at the joints.
Diagnosis
The exam may reveal a toe in which the near bone of the toe (proximal phalanx) is angled upward and the middle bone of the toe points in the opposite direction (plantar flexed). Toes may appear crooked or rotated. The involved joint may be painful when moved, or stiff. There may be areas of thickened skin (corns or calluses) on top of or between the toes, a callus may also be observed at the tip of the affected toe beneath the toenail. An attempt to passively correct the deformity will help elucidate the best treatment option as the examiner determines whether the toe is still flexible or not. It is advisable to assess palpable pulses, since their presence is associated with a good prognosis for healing after surgery. X-rays will demonstrate the contractures of the involved joints, as well as possible arthritic changes and bone enlargements (exostoses, spurs). X-rays of the involved foot are usually performed in a weight-bearing position.
Non Surgical Treatment
A number of approaches can be undertaken to the manage a hammer toe. It is important that any footwear advice is followed. The correct amount of space in the toe box will allow room for the toes to function without excessive pressure. If a corn is present, this will need to be treated. If the toe is still flexible, it may be possible to use splints or tape to try and correct the toe. Without correct fitting footwear, this is often unsuccessful. Padding is often used to get pressure off the toe to help the symptoms. If conservative treatment is unsuccessful at helping the symptoms, surgery is often a good option.
Surgical Treatment
The deformity is corrected in a variety of ways. There are actually a large number of procedures. The simplest procedure would involve a Tenotomy, the cutting of the tendon causing the deformity or a Tendon Lengthening procedure. These procedures are infrequently done, though, as the structural deformity (the arthritis and joint adaptation) is not addressed with these surgeries. Other soft-tissue procedures involve rebalancing the tendons around the joint. There are several techniques to do this, but the most common is probably the Girdlestone-Taylor procedure, which involves rerouting the tendons on the bottom of the toe up and over the toe where it sticks up, so that the tendon helps pull the toe downwards into proper alignment.
 Prevention
Prevention
Early Development. The first year of life is important for foot development. Parents should cover their babies' feet loosely, allowing plenty of opportunity for kicking and exercise. Change the child's position frequently. Children generally start to walk at 10 - 18 months. They should not be forced to start walking early. Wearing just socks or going barefoot indoors helps the foot develop normally and strongly and allows the toes to grasp. Going barefoot outside, however, increases the risk for injury and other conditions, such as plantar warts. Children should wear shoes that are light and flexible, and since their feet tend to perspire, their shoes should be made of materials that breathe. Replace footwear every few months as the child's feet grow. Footwear should never be handed down. Protect children's feet if they participate in high-impact sports.
What Are The Major Causes Of Bunions?
Overview
 Bunions, Corns, and Calluses are common foot ailments associated with improperly-fitted footwear. Please contact your family doctor or Podiatrist to ask them how Birkenstock footwear or arch supports can help treat your symptoms. Also, feel free to contact your local Birkenstock retailer about their healthy footwear recommendations. Birkenstock has many products that can help with Bunions, Corns, and Calluses. Bunions are a prominent bump on the inside of the foot around the big toe joint. Corns are an accumulation of dead skin cells usually found on the toes, forming thick hardened areas. They contain a cone-shaped core whose point can press on a nerve below causing pain. Calluses are also an accumulation of dead skin cells that harden and thicken over an area of the foot. They are the body?s defense mechanism against excessive pressure and friction. Calluses are normally found on the bottom of the foot, the heel, and/or the inside of the big toe.
Bunions, Corns, and Calluses are common foot ailments associated with improperly-fitted footwear. Please contact your family doctor or Podiatrist to ask them how Birkenstock footwear or arch supports can help treat your symptoms. Also, feel free to contact your local Birkenstock retailer about their healthy footwear recommendations. Birkenstock has many products that can help with Bunions, Corns, and Calluses. Bunions are a prominent bump on the inside of the foot around the big toe joint. Corns are an accumulation of dead skin cells usually found on the toes, forming thick hardened areas. They contain a cone-shaped core whose point can press on a nerve below causing pain. Calluses are also an accumulation of dead skin cells that harden and thicken over an area of the foot. They are the body?s defense mechanism against excessive pressure and friction. Calluses are normally found on the bottom of the foot, the heel, and/or the inside of the big toe.
Causes
Inflammatory joint diseases. Those who suffer from rheumatoid and psoriatic arthritis are at risk for bunions, although many times, those who suffer from bunions will mistakenly attribute the soreness in their feet to arthritis. Genetic and neuromuscular factors. Individuals with Down?s Syndrome are believed to be more prone to developing bunions; therefore, the gait and feet of such patients should be examined carefully and regularly so that any problems can be caught and treated early. Similarly, individuals of any age who have been diagnosed with Ehlers-Danlos or Marfan?s Syndrome, have also been shown to have a higher than average occurrence of bunions. Limb inequality. Individuals who have legs of unequal length often suffer from bunions on the longer limb due to the irregular mechanics of their walking or running gait.
Symptoms
The most common symptoms associated with this condition are pain on the side of the foot just behind the great toe. A red painful bump is usually present. Pain is usually brought on with walking or sports. Shoes don't cause bunions but will typically aggravate them. Stiff leather shoes or shoes with a tapered toe box are the prime offenders. This is why bunion pain is most common in women whose shoes have a pointed toe box. The bunion site will often be slightly swollen and red from the constant rubbing and irritation of a shoe. Occasionally, corns can develop between the 1st and 2nd toe from the pressure the toes rubbing against each other.
Diagnosis
Looking at the problem area on the foot is the best way to discover a bunion. If it has the shape characteristic of a bunion, this is the first hint of a problem. The doctor may also look at the shape of your leg, ankle, and foot while you are standing, and check the range of motion of your toe and joints by asking you to move your toes in different directions A closer examination with weight-bearing X-rays helps your doctor examine the actual bone structure at the joint and see how severe the problem is. A doctor may ask about the types of shoes you wear, sports or activities (e.g., ballet) you participate in, and whether or not you have had a recent injury. This information will help determine your treatment.
Non Surgical Treatment
Treatment may be surgical or non-surgical. The goal of non-surgical treatment is to relieve pressure on the foot and to prevent pressure sores and foot ulcers. This is accomplished by prescribing accommodative shoes with a wide toe box - sandals or extra depth shoes with soft moulded insoles. It may also be possible to relax the leather on shoes to make room for a bunion. 
Surgical Treatment
If nonsurgical treatment fails, you may want to consider surgery. Many studies have found that 85 to 90 percent of patients who undergo bunion surgery are satisfied with the results. Reasons that you may benefit from bunion surgery commonly include severe foot pain that limits your everyday activities, including walking and wearing reasonable shoes. You may find it hard to walk more than a few blocks (even in athletic shoes) without significant pain. Chronic big toe inflammation and swelling that doesn't improve with rest or medications. Toe deformity-a drifting in of your big toe toward the small toes. Toe stiffness-inability to bend and straighten your toe. Failure to obtain pain relief from nonsteroidal anti-inflammatory drugs. Their effectiveness in controlling toe pain varies greatly from person to person. Failure to substantially improve with other treatments such as a change in shoes and anti-inflammatory medication. As you explore bunion surgery, be aware that so-called "simple" or "minimal" surgical procedures are often inadequate "quick fixes" that can do more harm than good. And beware of unrealistic claims that surgery can give you a "perfect" foot. The goal of surgery is to relieve as much pain, and correct as much deformity as is realistically possible. It is not meant to be cosmetic.
Prevention
The simplest way to reduce your chance of developing foot bunion or bunionette problems is to wear good-fitting shoes. Avoid high heels as they push your feet forwards to the front of the shoe where they get squashed. Also avoid narrow fitting shoes, especially those that are pointed at the front with a narrow toe box as again, these place pressure through the toes pushing them inwards. Shoes should be comfortable and leave enough room for you to wiggle your toes. Remember, bunions rarely affect non-shoe wearing people. Exercising your feet can also help. By strengthening the foot muscles you can improve your foot position which can help reduce foot bunion problems. Simple exercises like picking up small objects with your toes can help.
Is Over-Pronation
Overpronation is a term that gets thrown around a lot by psuedo-experts and there is so much written online about it, that it can get very confusing to determine what is legitimate and what is not. Pronation is a normal motion of the foot that occurs when the ankle rolls inwards and the arch collapses. This is normal. Its not something evil. Overpronation is assumed to be when there is too much of it. There certainly is debate as to just how much is too much, as some people have large amounts and have no problems, other have small amounts and do have problems. It all comes down to individual differences and how much force is needed to stop the foot moving. The greater the force, regardless of the amounts of pronation, the more likely it is to be a problem. Some still like to debate if it is a problem or not. Some studies have shown that its not a problem and other studies have shown it is. If the data from all these studies are pooled, then the conclusion was that, yes, overpronation is a problem that was statistically significant, but it was only a small risk factor for problems. An associated finding of overpronation during a gait analysis is an abductory twist.

Causes
There may be several possible causes of over pronation. The condition may begin as early as birth. However, there are several more common explanations for the condition. First, wear and tear on the muscles throughout the foot, either from aging or repetitive strain, causes the muscles to weaken, thereby causing the foot to turn excessively inward. Also, standing or walking on high heels for an extended period of time also places strain and pressure on the foot which can weaken the tissue. Lastly, shoes play a very common factor in the development of over pronation. Shoes that fail to provide adequate support through the arch commonly lead to over pronation.
Symptoms
If you overpronate, your symptoms may include discomfort in the arch and sole of foot. Your foot may appear to turn outward at the ankle. Your shoes wear down faster on the medial (inner) side of your shoes. Pain in ankle, shins, knees, or hips, especially when walking or running.Unfortunately, overpronation can lead to additional problems with your feet, ankles, and knees. Runners in particular find that overpronation can lead to shin splints, tarsal tunnel syndrome, plantar fasciitis, compartment syndrome, achilles tendonitis, bunions (hallux valgus) patello femoral pain syndrome, heel spurs, metatarsalgia. You do not have to be a runner or athlete to suffer from overpronation. Flat feet can be inherited, and many people suffer from pain on a day-to-day basis. Flat feet can also be traumatic in nature and result from tendon damage over time. Wearing shoes that do not offer enough arch support can also contribute to overpronation.
Diagnosis
Do the wet foot test. Get your feet wet and walk along a paved surface or sand and look at the footprints you leave. If you have neutral feet you will see a print of the heel with a thin strip connecting to your forefoot, but if you're overpronating your foot print will look a bit like a giant blob with toes.
Non Surgical Treatment
Side Step with Opposite Reach. This exercise is designed to load the "bungee cord system" of the gluteal muscle and its opposite, latissimus dorsi muscle to keep the foot from overpronating. Because the opposite arm swings across the front leg when walking, this exercise creates tension in the muscles all the way from the front foot, across the back of the hips and back, to the fingers of the opposite hand. Movement Directions. Stand with left foot on top of the dome of the BT. (Note: For added balance, the right foot can tap on the ground, if needed). Reach right leg out to the side of the BT, and tap the ground while squatting down on the left side and reaching right arm across the left knee. Push down with left big toe while squatting. This activates the arch of the left foot and strengthens all the stabilizing muscles on the left side of the lower body. Return to starting position. Perform 8 to 10 repetitions on each leg.
Surgical Treatment
Subtalar Arthroereisis. The ankle and hindfoot bones/midfoot bones around the joint are fused, locking the bones in place and preventing all joint motion. This may also be done in combination with fusion at other joints. This is a very aggressive option usually reserved for extreme cases where no joint flexibility is present and/or the patient has severe arthritic changes in the joint.
Addressing Calcaneal Apophysitis
This condition is self limiting, it will go away when the two parts of bony growth join together, this is natural. Unfortunately, Sever's disease can be very painful and limit sport activity of the child while waiting for it to go away, so treatment is often advised to help relieve it. In a few cases of Sever's disease, the treatment is not successful and these children will be restricted in their activity levels until the two growth areas join, usually around the age of 16 years. There are no known long term complications associated with Sever's disease.
Causes
Apart from age, other factors that may contribute to developing Sever?s disease include physical activity, any form of exercise that is weight bearing through the legs or stresses the soft tissue can exacerbate the pain of the disease. External factors, for example, running on hard surfaces or wearing inappropriate shoes during sport. Overuse injury, very active children may repeatedly but subtly injure the bones, muscles and tendons of their feet and ankles. In time, the accumulated injuries cause symptoms.
Symptoms
The most prominent symptom of Sever's disease is heel pain which is usually aggravated by physical activity such as walking, running or jumping. The pain is localised to the posterior and plantar side of the heel over the calcaneal apophysis. Sometimes, the pain may be so severe that it may cause limping and interfere with physical performance in sports. External appearance of the heel is almost always normal, and signs of local disease such as edema, erythema (redness) are absent. The main diagnostic tool is pain on medial- lateral compression of the calcaneus in the area of growth plate, so called squeeze test. Foot radiographs are usually normal. Therefore the diagnosis of Sever's disease is primarily clinical.
Diagnosis
Sever condition is diagnosed by detecting the characteristic symptoms and signs above in the older children, particularly boys between 8 and 15 years of age. Sometimes X-ray testing can be helpful as it can occasionally demonstrate irregularity of the calcaneus bone at the point where the Achilles tendon attaches.
Non Surgical Treatment
The initial treatment is rest, relieve the pain and treat the underlying cause. The foot and ankle should be rested so that the apophysis it is not being continually ?injured?. A small heel (sorbothane heel insert) raise can used to raise the heel and take the stretch off the Achilles tendon. It may be sufficient to stop your child playing sport but some children require a short period of bed or couch rest. Some children find resting very difficult and require the use of braces or plasters or boots to slow them down. Using crutches is advised. Severs is usually caused by tight muscles. A stretching program should be followed usually supervised by a physiotherapist. The stretching program may need to be undertaken up to 5 times a day. If flat feet are a problems orthotics (insoles) should be used. The pain should be controlled by rest (limiting activity) and ice (icing the painful area 3-4 times a day - making sure the skin is not burnt), Simple pain killers can be used such as paracetamol as well as anti-inflammatory tablets and cream. Severs disease usually goes away with time. When your child stops growing, the pain and swelling should go away because the growing (weak) area fuses and becomes solid bone which is very strong.
Exercise
Stretching exercises can help. It is important that your child performs exercises to stretch the hamstring and calf muscles, and the tendons on the back of the leg. The child should do these stretches 2 or 3 times a day. Each stretch should be held for about 20 seconds. Both legs should be stretched, even if the pain is only in 1 heel. Your child also needs to do exercises to strengthen the muscles on the front of the shin. To do this, your child should sit on the floor, keeping his or her hurt leg straight. One end of a bungee cord or piece of rubber tubing is hooked around a table leg. The other end is hitched around the child's toes. The child then scoots back just far enough to stretch the cord. Next, the child slowly bends the foot toward his or her body. When the child cannot bend the foot any closer, he or she slowly points the foot in the opposite direction (toward the table). This exercise (15 repetitions of "foot curling") should be done about 3 times. The child should do this exercise routine a few times daily.
What Exactly Is Adult Aquired FlatFeet ?
Overview
For many adults, years of wear and tear on the feet can lead to a gradual and potentially debilitating collapse of the arch. However, a new treatment approach based on early surgical intervention is achieving a high rate of longterm success. Based on results of clinical studies of adults with flat feet, we now believe that reconstructive surgery in the early stages of the condition can prevent complications later on. Left untreated, the arch eventually will collapse, causing debilitating arthritis in the foot and ankle. At this end stage, surgical fusions are often required to stabilize the foot. 
Causes
Posterior tibial tendon dysfunction is the most common cause of acquired adult flatfoot. Sometimes this can be a result of specific trauma, but usually the tendon becomes injured from wear and tear over time. This is more prevalent in individuals with an inherited flat foot but excessive weight, age, and level of activity are also contributing factors.
Symptoms
Many patients with this condition have no pain or symptoms. When problems do arise, the good news is that acquired flatfoot treatment is often very effective. Initially, it will be important to rest and avoid activities that worsen the pain.
Diagnosis
First, both feet should be examined with the patient standing and the entire lower extremity visible. The foot should be inspected from above as well as from behind the patient, as valgus angulation of the hindfoot is best appreciated when the foot is viewed from behind. Johnson described the so-called more-toes sign: with more advanced deformity and abduction of the forefoot, more of the lateral toes become visible when the foot is viewed from behind. The single-limb heel-rise test is an excellent determinant of the function of the posterior tibial tendon. The patient is asked to attempt to rise onto the ball of one foot while the other foot is suspended off the floor. Under normal circumstances, the posterior tibial muscle, which inverts and stabilizes the hindfoot, is activated as the patient begins to rise onto the forefoot. The gastrocnemius-soleus muscle group then elevates the calcaneus, and the heel-rise is accomplished. With dysfunction of the posterior tibial tendon, however, inversion of the heel is weak, and either the heel remains in valgus or the patient is unable to rise onto the forefoot. If the patient can do a single-limb heel-rise, the limb may be stressed further by asking the patient to perform this maneuver repetitively.
Non surgical Treatment
Stage one deformities usually respond to conservative or non-surgical therapy such as anti-inflammatory medication, casting, functional orthotics or a foot ankle orthosis called a Richie Brace. If these modalities are unsuccessful surgery is warranted. 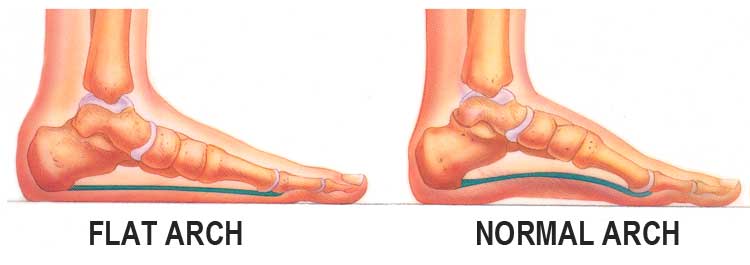
Surgical Treatment
Many operations are available for the treatment of dysfunction of the posterior tibial tendon after a thorough program of non-operative treatment has failed. The type of operation that is selected is determined by the age, weight, and level of activity of the patient as well as the extent of the deformity. The clinical stages outlined previously are a useful guide to operative care (Table I). In general, the clinician should perform the least invasive procedure that will decrease pain and improve function. One should consider the effects of each procedure, particularly those of arthrodesis, on the function of the rest of the foot and ankle.